Resistance to injection is part of the standard documentation procedure during nerve blocks and this documentation of resistance is merely subjective, and relies on the “learned feel” and experience of the provider.
The B-Smart pressure monitor is the first disposable manometer for objective monitoring of injection pressure during administration of peripheral nerve blocks (PNB). Monitoring opening injection pressure with B-Smart can help identify potentially unsafe injections before they start.
When the B-Smart monitor indicates high (> 15 psi) opening injection pressure, the needle can be repositioned and the injection resumed.
It’s objective pressure information, regardless of who performs the injection.
Take away the guess work: Provides a visual indication of injection pressure
Last line of defense: Monitoring pressure in real-time provides unbiased information to make more informed decisions on how to proceed with an injection
Objective documentation: A neutral and quantifiable method of monitoring and documenting injection pressure
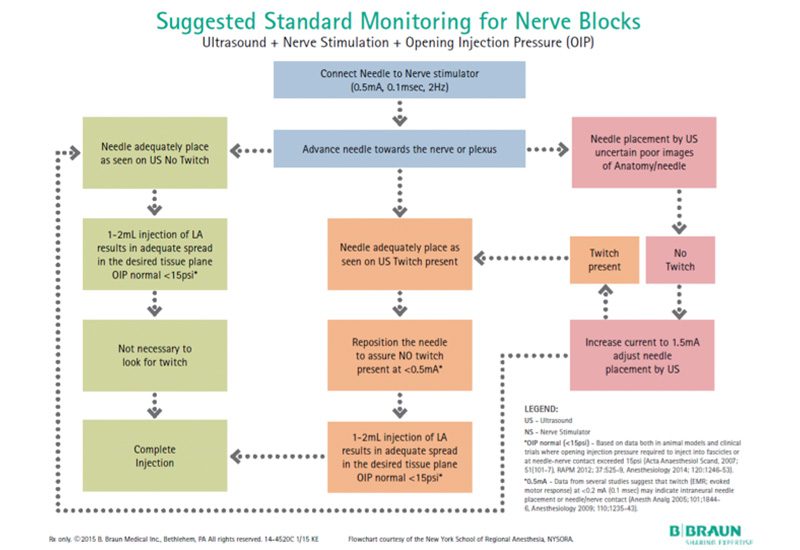
Injection Safety Monitoring Flow Chart
The typical sequence of events when performing nerve blocks using the multiple monitors is outlined in the flowchart below
Anatomy of a Nerve Injury
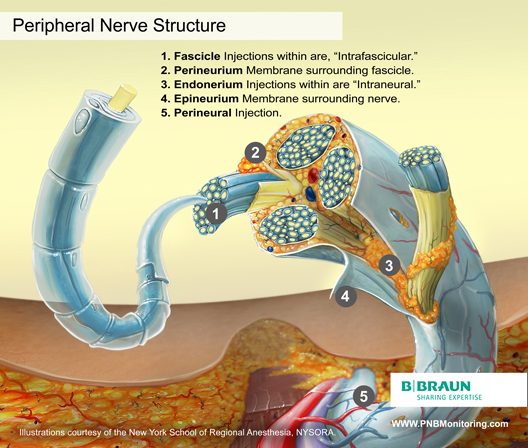
Peripheral Nerve Structure
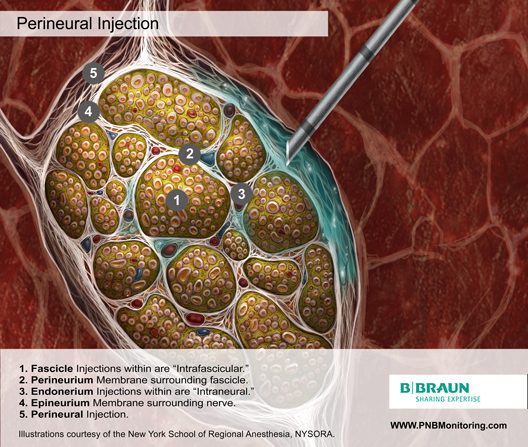
Knowledge of the functional histology of nerves is essential to understanding the consequences of intraneural injection. Nerves are made up of fascicles supported and enveloped by perineurium and a loose collection of collagen fibers termed the epineurium. The epineurium is easily permeable and carries the nutritive vessels of larger nerves. Each fascicle is made up of bundles of nerve fibers (axons) and their associated Schwann cells held together by a tough squamous epithelial sheath called the perineurium, which acts as a semipermeable barrier to local anesthetics. The nerve fibers are supported within the perineurium by a delicate connective tissue matrix called the endoneurium, which contains capillaries that arise from the larger epineurial vessels.
The etiology of perioperative nerve injury is complex and multifactorial.7 Postulated surgical mechanisms include:
- Compression due to pneumatic tourniquets or casts, stretch injuries from positioning
- Surgical injuries
Postulated anesthesia related mechanisms include:
- Chemical neurotoxicity from either the local anesthetic solution itself or from vasoconstrictive additives such as epinephrine
- Mechanical injury from needle-nerve contact and/or puncture.8
- Rupturing of the fascicle as a result of a high injection pressure. 29
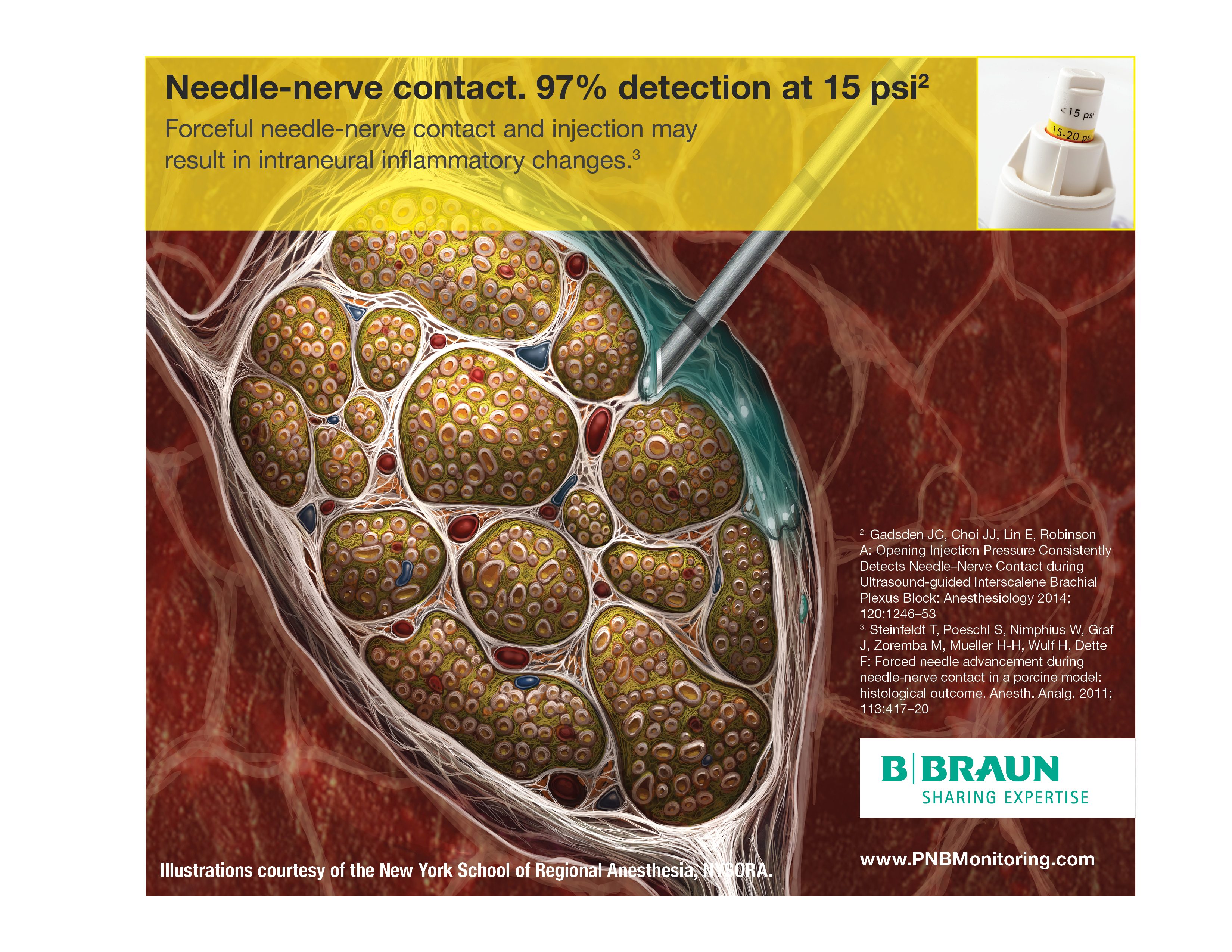
Strategies aimed at preventing nerve injury include using the lowest effective concentration of local anesthetic, taking care with limb positioning, and cast application, and the use of meticulous surgical technique. However, since mechanical injury from the needle and the affects of high injection pressure remains the most likely causative mechanism following a peripheral nerve block, much effort has been directed at preventing harmful needle-nerve contact & detecting high pressures through the use of multiple monitors.
Nerve Injections
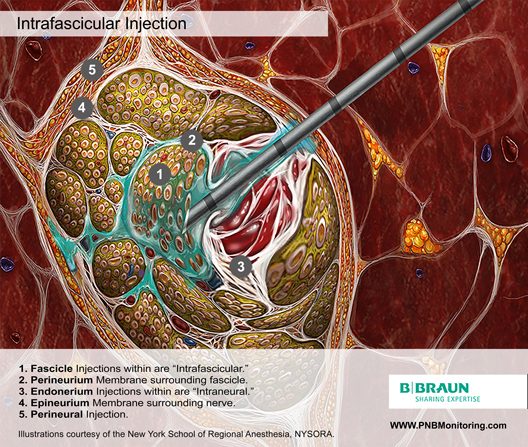
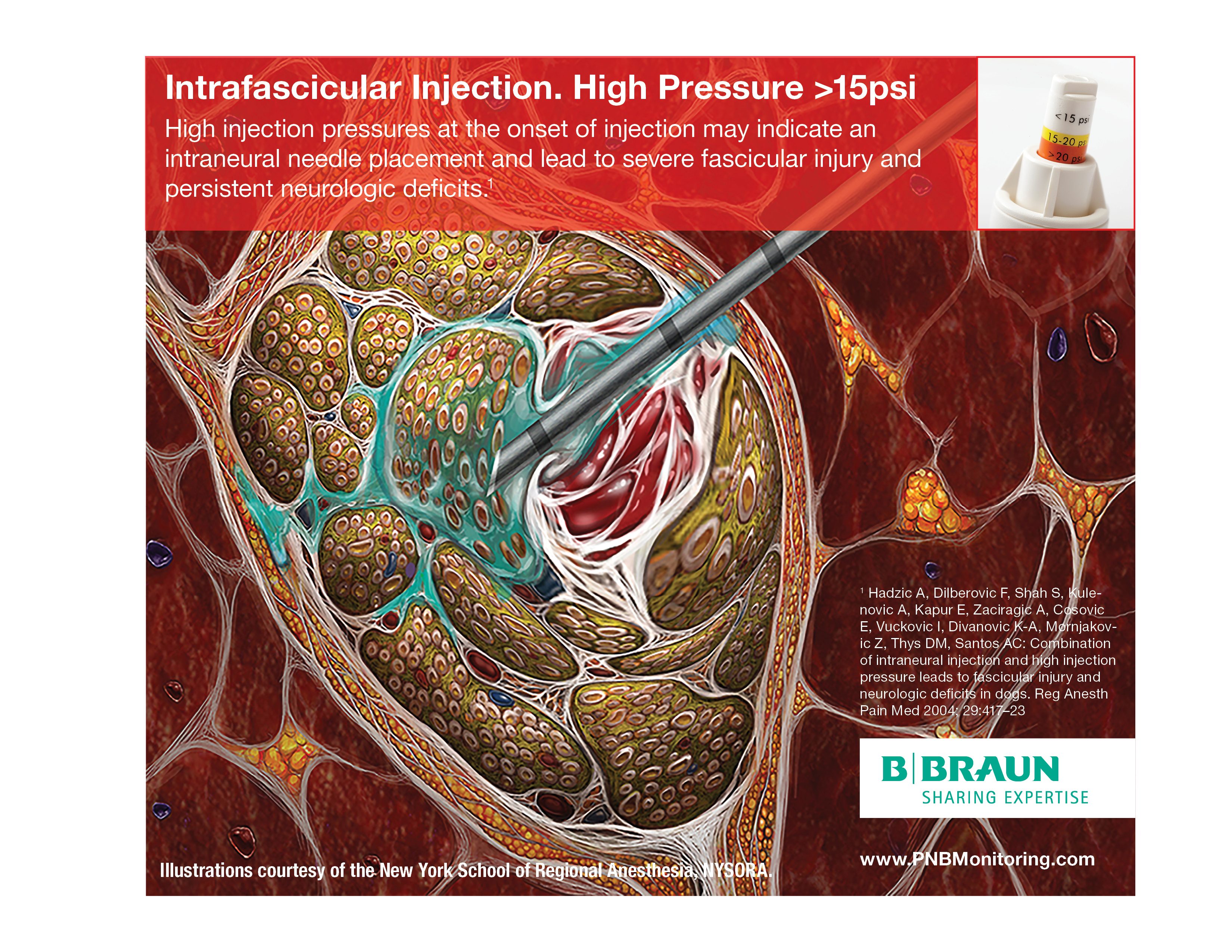
Intrafascicular Injection
It is well established that injection of even very small amounts of local anesthetic within the fascicle can lead to widespread axonal degeneration and permanent neural damage in animals, whereas extra-fascicular injection does not disrupt the normal nerve architecture. 9,10
Fortunately, the incidence of intrafasicular injection is rare, probably because the tough perineurium prevents needle advancement.
The risk of an intrafascicular injection differs from site to site in the peripheral nervous system, and it correlates with the cross‐sectional fascicle‐connective tissue ratio. For example, the sciatic nerve at the popliteal fossa contains a relatively high proportion of loose connective tissue compared to fascicles, which corresponds with its low incidence of post-PNB neuropathy.11 By contrast, the brachial plexus at the level of the trunks is nearly all neural tissue, a needle entering the nerve here is more likely to encounter a fascicle on its trajectory that may contribute to the disproportionately higher rate of postoperative neuropathy following PNB with interscalene blocks.12
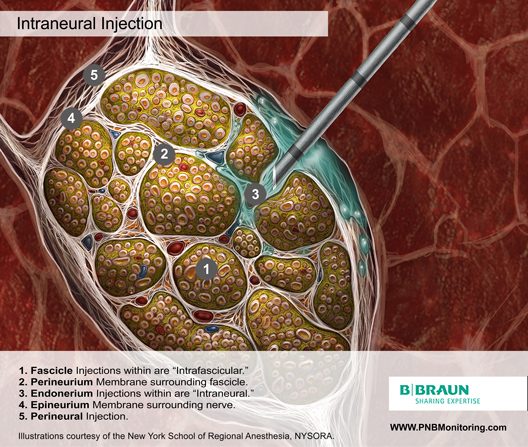
Intraneural Injection
In 2006, Bigeleisen published a series of axillary brachial plexus blocks performed on 22 patients undergoing thumb surgery.13 Using ultrasound guidance, the authors deliberately placed the needle intraneurally and injected 2 to 3 mL of local anesthetic, which resulted in 72 intraneural injections as evidenced by nerve swelling. Despite the common occurrence of paresthesia or dysesthesia (66 times), none of the patients developed an overt neurologic deficit up to 6 months postoperatively.
Similarly, Robards et al studied 24 patients receiving sciatic nerve blocks in the popliteal fossa using both nerve stimulation and ultrasound guidance.14 The end point for needle advancement was a motor response using a current intensity of 0.2 to 0.5 mA, or an apparent intraneural needle tip location, whichever came first. There was no postoperative neurologic dysfunction.
While interesting, these results are far from reassuring to the provider given the small number of subjects and relatively low incidence of PONS, and these data should not be interpreted as evidence that intraneural injections are safe. Intraneural injection observed with ultrasound has been reported to lead to long-term injury.15 Moreover, there are fine inter-fascicular neural connections and blood vessels within the epineurium that are likely easily damaged with intraneural needling, even if the fascicles themselves are not penetrated.15
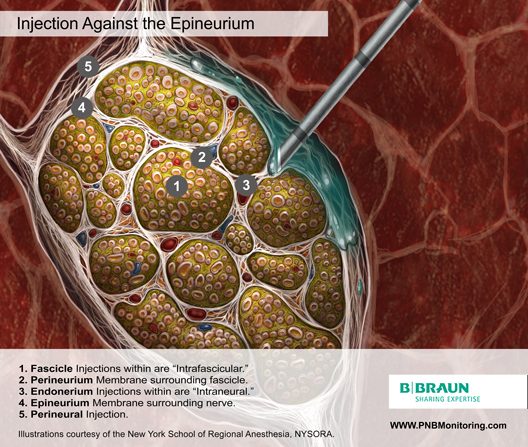
Injection Against the Epinuerium
Injecting local anesthetic while the needle tip is apposed to the epineurium may present a real danger of intraneural deposition of the injectate, since part or all of the needle opening may be embedded within this layer. Even if injection is not performed, simply contacting the epineurium with the needle and displacing the nerve has been shown to cause injury.17
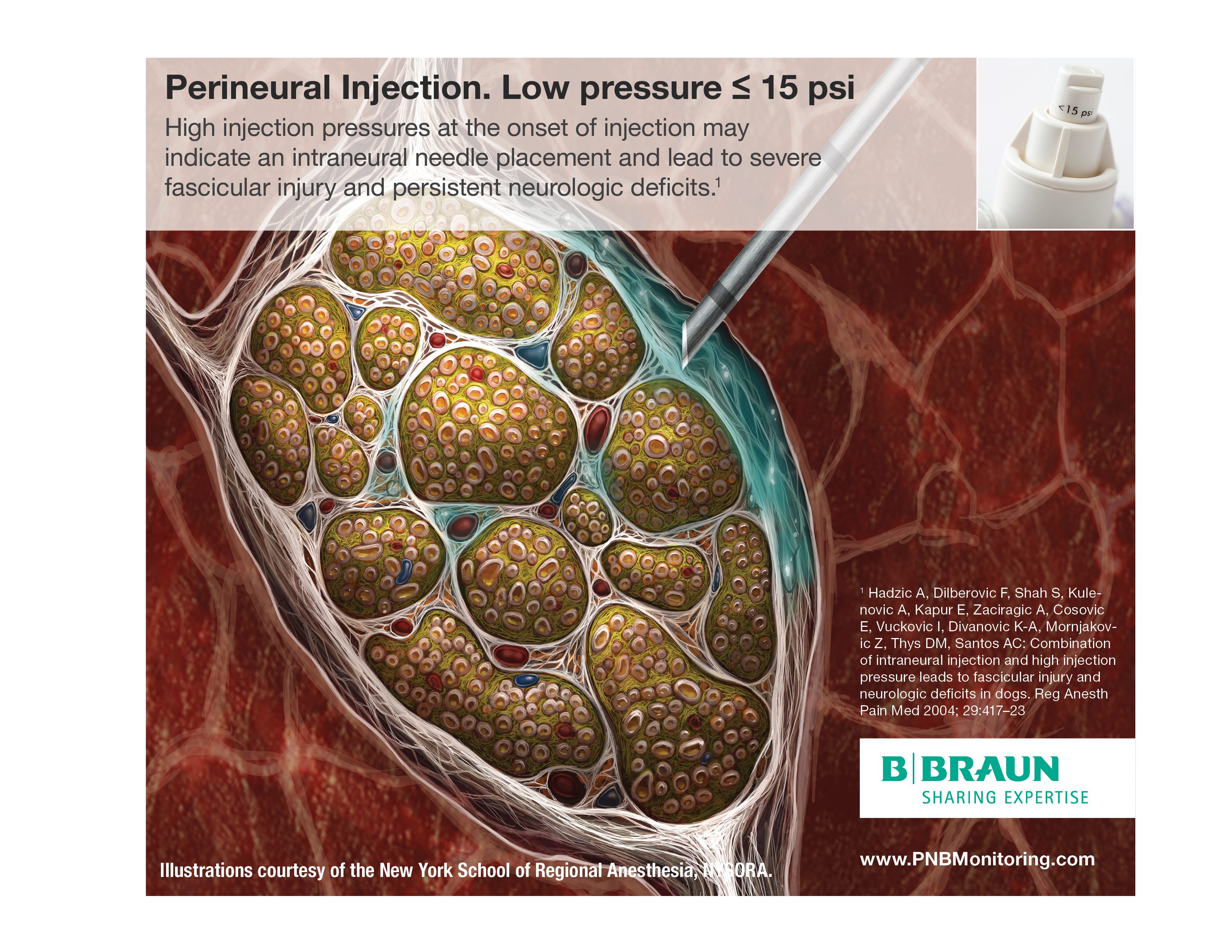
Perineural Injection
Most regional anesthesiologists agree that injection of local anesthetic into the nerve is a risk factor for injury, and that extra-neural deposition minimizes the potential for an intrafascicular injection.18
The Two Phases of Injection
Implications for objective injection pressure monitoring.
Isostatic Phase (opening pressure to start the flow)
There is no flow at the tip of the needle. A certain (opening) pressure must be reached within the syringe-tubing-needle system in order to INITIATE the injection into a tissue compartment. During this phase the pressure is equal throughout the entire closed system (including the needle opening: Pascal’s law)32 and is therefore not impacted by needle or syringe size or the speed of injection.
Aborting injection when opening pressure is above (>15 psi) can prevent the injection against the nerve, into a fascicle, or into other undesired low compliance tissues (e.g., tendons, tissue fascicle) before it occurs. In this case, a slight withdrawal of the needle and reconfirmation of the needle tip position is suggested before initiating injection.
Dynamic Phase (during the flow)
Once the opening pressure is overcome the injection is initiated, the injection pressure becomes affected by the rate of injection and the flow characteristics of the fluid passages including needle or syringe size and speed of injection (Bernoulli’s principle)33
Regardless, avoidance of high pressures using an objective monitoring device can prevent too rapid, forceful injection.
Monitoring for opening pressure becomes relevant any time the operator repositions the needle for additional injection.
7. Gadsden J, Gratenstein K, Hadzic A: Intraneural Injection and Peripheral Nerve Injury: International Anesthesiology Clinics 2010; 48:107–15
8. Hogan QH: Pathophysiology of peripheral nerve injury during regional anesthesia. Reg Anesth Pain Med 2008; 33:435–41
9. Selander D, Brattsand R, Lundborg G, Nordborg C, Olsson Y. Local anesthetics: importance of mode of application, concentration and adrenaline for the appearance of nerve lesions. An experimental study of axonal degeneration and barrier damage after intrafascicular injection or topical application of bupivacaine. Acta Anaesthesiol Scand. 1979; 23(2): 127-136.
10.Gentili F, Hudson AR, Hunter D, Kline DG. Nerve injection injury with local anesthetic agents: a light and electron microscopic, fluorescent microscopic, and horseradish peroxidase study. Neurosurgery. 1980; 6(3): 263-272.
11.Moayeri N, Groen GJ. Differences in quantitative architecture of sciatic nerve may explain differences in potential vulnerability to nerve injury, onset time, and minimum effective anesthetic volume. Anesthesiology. 2009l 111(5):1128-1134.
12.Liu SS, Zays VM, Gordon MA, et al. A prospective, randomized, controlled trial comparing ultrasound versus nerve stimulator guidance for interscalene block for ambulatory shoulder surgery for postoperative neurological symptoms. Anesth Analg. 2009; 109(1): 265-271.
13.Bigeleisen PE, Nerve puncture and apparent intraneural injection during ultrasound-guided axillary block does not invariably result in a neurologic injury. Anesthesiology. 2006; 105(4): 779-783.
14.Robards C, Hadzic A, Somasundaram L, Iwata T, Gadsden J, Xu D, Sala-Blanch X: Intraneural injection with low-current stimulation during popliteal sciatic nerve block. Anesth. Analg 2009; 109:673–7
15.Cohen JM, Gray AT: Functional deficits after intraneural injection during interscalene block. Reg Anesth Pain Med 2010; 35:397–9
17.Steinfeldt T, Poeschl S, Nimphius W, Graf J, Zoremba M, Mueller H-H, Wulf H, Dette F: Forced needle advancement during needle-nerve contact in a porcine model: histological outcome. Anesth. Analg. 2011; 113:417–20
18.Farber SJ, Saheb-Al-Zamani M, Zieske L, Laurido-Soto O, Bery A, Hunter D, Johnson P, Mackinnon SE: Peripheral nerve injury after local anesthetic injection. Anesth. Analg. 2013; 117:731–9
29.Claudio R, Hadzic A, Shih H, Vloka JD, Castro J, Koscielniak-Nielsen Z, Thys DM, Santos AC: Injection pressures by anesthesiologists during simulated peripheral nerve block. Reg Anesth Pain Med 2004; 29:201–5
32.Billings BH et a. : Fundamental concepts of mechanics. In American institute of physics.3rd edition. Edited by Gray DE. McGraw-Hill, New York, NY, 1972, pp 2-14.
33.Marchioro C et al: Conservation laws. In Mathematical theory of incompressible nonviscous fluids. Edited by John F, Marsden JE, Sirovich L. Springer-Verlag, New York, NY, 1994, pp 24-5.